Symptoms
The symptoms of pleural effusion depend on how quickly the fluid accumulates and how much is present. Common symptoms include:
- Shortness of breath, especially during physical activity or while lying down.
- Chest pain, often sharp and worsened by deep breathing (pleuritic pain).
- Dry cough, usually without signs of infection.
- In more severe cases, patients may feel a sense of heaviness or pressure in the chest.
During physical examination, the doctor may detect decreased breath sounds or dullness upon percussion on the affected side.
Diagnosis
Diagnosis involves a combination of clinical assessment and imaging studies:
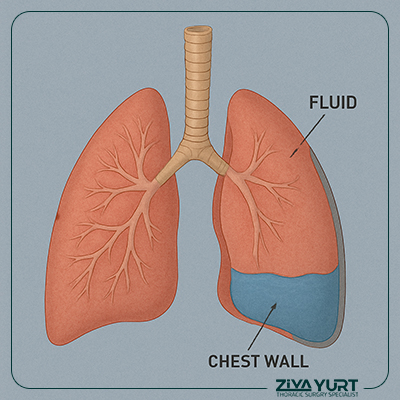
- Chest X-ray: Commonly used to detect fluid collection, typically at the lung bases.
- Ultrasound: Helps in precisely locating the fluid and guiding thoracentesis (fluid removal).
- CT scan: Useful in complex or recurrent cases to identify the underlying cause, such as a tumor.
- Thoracentesis (pleural tap): A key diagnostic procedure where fluid is drawn from the pleural space and analyzed for protein content, cell types, infectious organisms, or cancer cells.
The analysis helps differentiate between transudative effusions (usually from systemic conditions like heart failure) and exudative effusions (typically caused by infection, inflammation, or malignancy).
Treatment
Treatment focuses on managing the underlying cause and relieving symptoms:
- In cases of heart failure, diuretics are used to reduce fluid accumulation.
- If the cause is a bacterial infection, antibiotic therapy is essential, and fluid drainage may be necessary if there is significant accumulation or empyema (pus in the pleural space).
- Tuberculosis-related effusions require long-term anti-tuberculous medications.
- For malignant effusions, treatment may include chemotherapy, radiotherapy, or pleural drainage to relieve symptoms.
- In recurrent effusions, pleurodesis—a procedure that adheres the lung to the chest wall—may be performed to prevent fluid reaccumulation.
Follow-Up and Prevention
After initial treatment, patients should be monitored through regular clinical exams and imaging to ensure resolution and detect recurrence. Treating the primary disease effectively is crucial in preventing future pleural effusions.
In cases of advanced cancer or chronic illness, long-term management and periodic fluid drainage may be required. Accurate diagnosis and timely treatment of pleural effusion significantly improve respiratory comfort and overall quality of life for affected patients.