Symptoms
The symptoms vary depending on the size of the pneumothorax and how rapidly it develops. Common signs and symptoms include:
- Sudden sharp chest pain, typically on one side, which worsens with deep breathing or coughing.
- Shortness of breath, ranging from mild to severe.
- Rapid breathing and increased heart rate.
- A feeling of tightness in the chest or dizziness, especially in larger pneumothoraces.
- In tension pneumothorax, there may be low blood pressure, bluish discoloration of the lips (cyanosis), and loss of consciousness—all signs of a life-threatening emergency.
Diagnosis
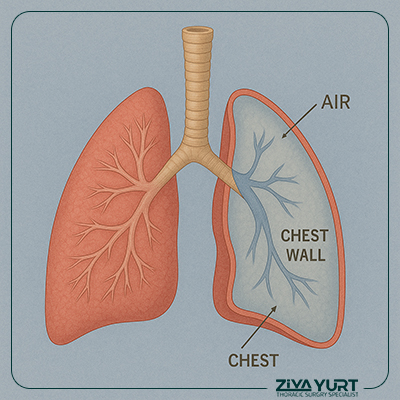
Diagnosis typically begins with a thorough clinical examination. The doctor may detect decreased breath sounds on one side of the chest. To confirm the diagnosis, imaging studies are used:
- Chest X-ray is the most common and reliable initial test to identify the presence of air in the pleural space.
- CT scan provides more detailed imaging and is useful in complicated or recurrent cases.
- In cases of tension pneumothorax, diagnosis is primarily clinical and should not be delayed for imaging; immediate treatment is often necessary.
Treatment
Treatment depends on the type, size, and severity of the pneumothorax, as well as the patient’s overall condition:
- In mild cases of spontaneous pneumothorax without significant symptoms, observation and supplemental oxygen may be sufficient, as the air is gradually reabsorbed and the lung re-expands naturally.
- In larger or symptomatic cases, a chest tube (thoracostomy) may be inserted to evacuate air and allow the lung to reinflate.
- In a tension pneumothorax, immediate decompression is critical. This is typically performed by inserting a large-bore needle or chest tube to release trapped air and relieve pressure on the heart and lungs.
- Surgical intervention may be required in recurrent cases or when pneumothorax is associated with underlying lung disease. Procedures include bullectomy (removal of air sacs) or pleurodesis, where the lung is fused to the chest wall to prevent recurrence.
Follow-Up and Prevention
After treatment, follow-up is essential to ensure full lung re-expansion and to monitor for recurrence. Patients are often advised to avoid air travel or deep-sea diving for a period of time, as pressure changes can trigger a relapse.
Smoking cessation is crucial, particularly in patients who have experienced a spontaneous pneumothorax, as smoking increases the risk of recurrence. In patients with underlying lung conditions, managing the root cause is key to preventing future episodes.
Early recognition and prompt management of pneumothorax are vital for preventing complications and ensuring a full recovery of lung function.